# RKS: VEGETARIANS & VEGANS (III): Excessive Carbs - Complications Beyond Diabetes
# RKS: VEGETARIANS & VEGANS (III)
EXCESSIVE CARBS - COMPLICATIONS BEYOND DIABETES
CASCADING EFFECTS OF CARBS IN DIET
VEGETARIANS & VEGANS - BE WARY
Dear Reader,
The previous blog of January 2024 was elaborative in linking Type 2 Diabetes Mellitus (T2DM) with excessive carbohydrates (carbs) intake. But surprisingly and sadly that is not the end of matter. The plunder by carbs, once initiated, progresses unbridled.
Medical jargon apart, it needs to be fathomed and ingested and registered that carbs consumption amongst especially the vegetarians and vegans needs to be curtailed and / or replaced with some other macronutrient i.e. either proteins and / or fats.
CLARITY ON GLUCOSE LEVELS & ESTIMATIONS
NORMAL GLUCOSE CONCENTRATIONS
The normal fasting blood glucose concentrations are considered, as based on guidelines of:
The normal fasting blood glucose concentrations are considered, as based on guidelines of:
- World Health Organization (WHO): 70 mg/dL (3.9 mmol/L) to 100 mg/dL (5.6 mmol/L)
- American Association of Clinical Endocrinologists (AACE): 70 mg/dL (3.9 mmol/L) to 110 mg/dL (6.1 mmol/L)
- World Health Organization (WHO): 70 mg/dL (3.9 mmol/L) to 100 mg/dL (5.6 mmol/L)
- American Association of Clinical Endocrinologists (AACE): 70 mg/dL (3.9 mmol/L) to 110 mg/dL (6.1 mmol/L)
In a healthy person the insulin is secreted from pancreas (endogenous insulin) whenever food is consumed. This insulin produced within body starts working post-meal and removes all the additional carbs from the blood that has entered via the food consumed. The insulin levels rise immediately, peak at one hour and persist for another one hour and the blood sugar level is restored to normal fasting concentrations within this time-frame of 2 hours post-eating.
Thus, any reading above 100 mg/dL (5.6 mmol/L) whether for fasting or 2 hours post-food (prandial) (PP) is considered as excess carbs present in blood and the individual is labelled as hyperglycemic.
In an hyperglycemic individual, the corresponding indicative fasting plasma glucose levels are:
- Pre-diabetes: 100-125 mg/dL
- T2DM: >125 mg/dL
As per the American Diabetes Association (ADA) the glycosylated hemoglobin (HbA1c or A1c) (a widely popular and a well-known marker of average 3 months blood glucose) indicative of hyperglycemia could be considered as:
- Pre-diabetes: 5.7-6.4% [117 mg/dL (6.5 mmol/dL) - 137 mg/dL (7.6 mmol/dL)]
- T2DM: >6.4%
Do these figures specified by standard guidelines, and considered as a benchmark to control blood glucose by health professionals, actually correlate with negating consequences of T2DM should be the one question that one needs to dwell upon.
GUIDELINES SET FOR T2DM CONTROL
For T2DM control, as per ADA: (http://diabetesed.net/wp-content/uploads/2017/12/2018-ADA-Standards-of-Care.pdf)
- Stringent goal: <6.5% [140 mg/dL (7.8 mmol/L)]
- Reasonable goal: <7% [154 mg/dL (8.6 mmol/L]
- Less stringent control: <8% [183 mg/dL (10 mmol/dL)]
Although the current ADA guidelines suggest A1c criteria as <7% for fine-tuning dose of diabetes pills, the same could preferably be reset at a more stringent control of <6.5% provided the risk of lowering blood glucose to lesser than 70 mg/dL (and causing hypoglycemia) has been suitably negated by following strict diet routines such as meal timings as well as preferring drugs that do not easily precipitate episodes of hypoglycemia.
All the goals for controlling blood glucose in T2DM prophesies, including the ADA guidelines, keeping plasma glucose above the normal individual's fasting level of 110 mg/dL. Herein lies the catch and the key to future health complications because of not controlling blood sugar strictly akin to concentrations present in normal non-diabetic individuals.
In a healthy person the insulin is secreted from pancreas (endogenous insulin) whenever food is consumed. This insulin produced within body starts working post-meal and removes all the additional carbs from the blood that has entered via the food consumed. The insulin levels rise immediately, peak at one hour and persist for another one hour and the blood sugar level is restored to normal fasting concentrations within this time-frame of 2 hours post-eating.
Thus, any reading above 100 mg/dL (5.6 mmol/L) whether for fasting or 2 hours post-food (prandial) (PP) is considered as excess carbs present in blood and the individual is labelled as hyperglycemic.
In an hyperglycemic individual, the corresponding indicative fasting plasma glucose levels are:
- Pre-diabetes: 100-125 mg/dL
- T2DM: >125 mg/dL
As per the American Diabetes Association (ADA) the glycosylated hemoglobin (HbA1c or A1c) (a widely popular and a well-known marker of average 3 months blood glucose) indicative of hyperglycemia could be considered as:
- Pre-diabetes: 5.7-6.4% [117 mg/dL (6.5 mmol/dL) - 137 mg/dL (7.6 mmol/dL)]
- T2DM: >6.4%
Do these figures specified by standard guidelines, and considered as a benchmark to control blood glucose by health professionals, actually correlate with negating consequences of T2DM should be the one question that one needs to dwell upon.
GUIDELINES SET FOR T2DM CONTROL
For T2DM control, as per ADA: (http://diabetesed.net/wp-content/uploads/2017/12/2018-ADA-Standards-of-Care.pdf)
- Stringent goal: <6.5% [140 mg/dL (7.8 mmol/L)]
- Reasonable goal: <7% [154 mg/dL (8.6 mmol/L]
- Less stringent control: <8% [183 mg/dL (10 mmol/dL)]
Although the current ADA guidelines suggest A1c criteria as <7% for fine-tuning dose of diabetes pills, the same could preferably be reset at a more stringent control of <6.5% provided the risk of lowering blood glucose to lesser than 70 mg/dL (and causing hypoglycemia) has been suitably negated by following strict diet routines such as meal timings as well as preferring drugs that do not easily precipitate episodes of hypoglycemia.
All the goals for controlling blood glucose in T2DM prophesies, including the ADA guidelines, keeping plasma glucose above the normal individual's fasting level of 110 mg/dL. Herein lies the catch and the key to future health complications because of not controlling blood sugar strictly akin to concentrations present in normal non-diabetic individuals.
THE LINK BETWEEN HIGH GLUCOSE & T2DM COMPLICATIONS
UNCONTROLLED DIABETES RAMPAGES THE BODY
T2DM is universally known, including to the layman, that it can ultimately affect the nerves, heart, brain, eyes and kidneys. These incidence of these complications are directly co-related to the levels of A1c maintained.
Fig: Varying A1c levels and relative risk of T2DM complications.
CLASSIFICATION OF T2DM COMPLICATIONS
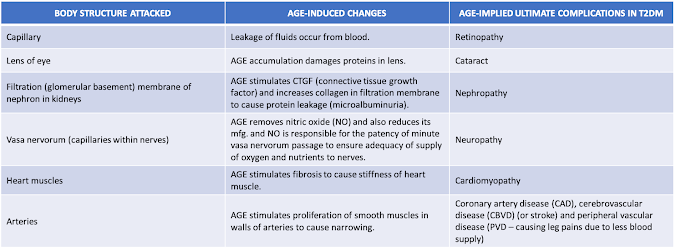
T2DM complications entail damaging blood vessels (angiopathy) which include both the microvascular (involving smaller vessels, such as capillaries) and macrovascular (involving the large vessels, such as arteries and veins) angiopathies.
- Microangiopathies damage to nerves, eyes and kidneys.
- Macroangiopathies contribute to diabetic foot (with gangrene possibilities) and also cause damage brain and heart.
Fig: Microvascular vs macrovascular complications of T2DM.
The changes caused are ultimately in the lining layer, called endothelium, of each of the 3 blood vessels in the body. The damage to the endothelium is the torch bearer of T2DM complications, including causing narrowing of arteries in macroangiopathies.
ANGIOPATHY MECHANISMS IN T2DM COMPLICATIONS
The mechanisms involved in chronic hyperglycemia precipitating diabetic vascular complications are primarily 3:
- Production of advanced glycation end products (AGE)
- Abnormal activation of signalling cascades [such as protein kinase C (PKC)]
- Elevated production of reactive oxygen species (ROS)
AGE
Advanced glycation end products (AGEs) are a family of compounds that are produced when sugars interact with proteins or lipids (fats). Roasting and broiling food at high temperatures is a common practice in cooking and these high temperatures facilitate formation of over 3 dozen known AGEs. These compounds play a very important role by giving special aroma, color and taste to different foods. Foods highest in AGEs include meat, certain cheeses, fried eggs, butter, mayonnaise, oils and nuts; fried foods and highly processed products also contain high levels. Examples of AGEs in food include Nϵ-carboxymethyl-lysine (CML), Nϵ-carboxyethyl-lysine (CEL), pyrraline, crossline, pentosidine, GOLD and MOLD (imidazolium cross-link derived from glyoxal / methylglyoxal and lysine-lysine).
As far as T2DM is concerned the elevated levels of glucose beyond 110 mg/dL commence interacting with various proteins such as:
- Proteins in blood: albumin (constitute 50% of plasma proteins), globulin (35%), fibrinogen (4%)
- Protein in blood vessel wall: collagen
When the excess glucose in T2DM combines with any of the above it forms AGEs. For precipitating changes in various cells and tissues, there is a receptor (RAGE) for AGE required to interact with. The RAGE are present in:
- Tissues: heart, lung, skeletal muscle and blood vessel wall
- Cells: nerve cell (neurons), brain cells (microglia, astrocytes, pericytes), blood vessel cells (endothelial cells, smooth muscle cells) and cells in blood (monocytes/macrophages and lymphocytes)
The consequences of AGE combining with RAGE is the basis of microvascular and macrovascular complications of T2DM.
Hence, AGEs affect the small as well as the large blood vessels over a period of time.
ABNORMAL SIGNALING MECHANISMS
To adapt to changing environments, cells must signal, and signalling requires messengers. Filling this role, calcium ions (Ca2+) have come to rule cell signalling. There are small pumps which either push:
- ATPase pump: Push Ca2+ in cell into their stores [called endoplasmic reticulum (ER)].
- PMCA pump: Push Ca2+ in cell out into blood.
An enzyme called protein kinase C (PKC) influences the Ca2+ release or otherwise. Enhanced PKC activity, as in uncontrolled glucose levels, loosens the junction in-between 2 cells of the capillary’s inner lining. As a result, the endothelium becomes leaky and contributes to the microvascular complications of T2DM like retinopathy and nephropathy. Even the NO production is compromised by PKC excess activity and nerve damage hastened.
ROS
The ROS are the major types of free oxygen radicals produced in humans. Usually ROS are continuously removed by antioxidants. The imbalance between production and destruction of free radicals is indeed defined as oxidative stress.
There are 3 ways by which ROS levels rise in T2DM:
- HYPERGLYCEMIA: Usually the carbs consumed enter the mitochondria to be converted into chemical energy in the form of adenosine triphosphate (ATP). During the process of ATP manufacturing (mfg.) [via the electron transfer chain (ETC)] ROS are liberated and neutralized effectively by the antioxidant enzymes given by God. However, in a not strictly controlled diabetic when there are excess carbs fed to the ETC, there is a large amount of ROS generated and all of these cannot be effectively negated by the limited antioxidants available in body. Hyperglycemia also decreases NO and this in turn leads to production of ROS. As a result of ROS burden increase in T2DM there is resultant oxidative stress.
- PKC STIMULATION: Activation of PKC also produces excess ROS by activation of an enzyme called NAD(P)H oxidase [nicotinamide adenine dinucleotide phosphate]. Oxidation of this later enzyme is the main mechanism of generating ROS.
- AGEs: The NAD(P)H oxidase enzyme itself is stimulated by AGEs and its further oxidation by PKC releases ROS.
ROS causes the complications of T2DM in two ways:
- Indirectly by increasing insulin resistance.
- Directly by damaging tissues of target organs affected due to diabetes.
ROS also destroys the beta cells in pancreas producing insulin over a period of years if the hyperglycemia persists unchecked.
ROS & INSULIN RESISTANCE
When insulin combines with its receptor a signal is initiated which enables a protein called GLUT-4 to be transferred to the wall of the cell and enable to open the ‘gate’ to allow glucose entry from the blood to within the tissues for 30-60 minutes. When this mechanism is prevented the phenomenon is called insulin resistance since the insulin is not able to drive away the excess glucose from the blood. ROS precipitates insulin resistance by:
- Interrupting with the signalling mechanism stimulating translocation of GLUT-4.
- Guiding the GLUT-4 proteins towards the lysosomes (waste paper baskets inside the cell) instead of to the outer cell membrane – glucose have no gates opened to enter.
ROS preferentially makes available GLUT-4 on surface of fat cells (adipocytes) to divert entry of excess glucose into liver, instead of muscles. After the glycogen stores of 100 gms in liver are replenished, the excess glucose is converted to triglycerides (another form of lipids). Seeing the glucose being removed from blood effectively, the pancreas mfg. more insulin and more carbs are converted preferentially to triglycerides since the liver cells exhibit more sensitivity to insulin’s action in comparison to the muscles. The resultant abnormally large quantities of converted triglycerides in hepatocytes (liver cells) precipitates the well-known syndrome of fatty liver in insulin resistance.
ROS & TISSUE / ORGAN DAMAGE
ROS damage the various organs and tissues known to be affected as a result of complications in an uncontrolled diabetic in many ways:- Diabetic neuropathy: ROS destroys the mitochondria of the nerve cells and reduce ATP generation. As a result, the nerve fibres lose their normal signalling abilities and this initiates diabetic neuropathy. Over a period of time, the myelin covering of the nerves is also destroyed by ROS.
- Diabetic foot: Loss of sensation on account of neuropathy of the nerves supplying the legs results in unappreciated damage to the foot to result in repeated wounds which also do not properly heal to due deficient blood supply (on account of PVD) – typically called diabetic foot.
- Diabetic retinopathy: The high amounts of fats present in retina are attacked by ROS to cause inflammation - retinopathy. Thereafter, the ROS in the backside chamber (behind the lens - vitreous humor) promote fibrous tissue to replace the retinal structure.
- Diabetic cardiomyopathy: ROS combines with protein in muscle fibres that cause contraction of heart. As a result of the distorted muscle proteins, following damage by ROS, the heart loses its normal contractility abilities and this leads to cardiomyopathy.
- Diabetic heart / brain disease & PVD: ROS damages the bad cholesterol (LDL-C - low density lipoprotein cholesterol) to form oxidized LDL. These are damaged LDL particles who have preferential ability to transfer their cholesterol to inside the walls of arteries. As a result, there is build-up of cholesterol plaques and the resultant narrowing compromises the blood flow in the macrovessels of the heart (diabetic ischemic heart disease), brain (diabetic CBVD) and legs (PVD).
- Diabetic nephropathy: ROS promote inflammation and fibrosis of kidney to first affect function and eventually destroy its normal structure by replacing it with fibrous issue.
ARE UNCONTROLLED DIABETES COMPLICATIONS A REAL THREAT?!
Most will not be spared of the complications of T2DM if the blood glucose is left uncontrolled and ignored.
Graph: The incidence of important complications of uncontrolled T2DM over a period of time.
Thus the hyperglycemia, in those not strictly controlling their blood glucose, in T2DM leads to:
- Peaking of nerve damage within 6-10 years in 40-45% of diabetics.
- Spurt in retinopathy and heart disease in 6-10 years.
- Slow progressive damage to blood vessels of legs (PVD) and kidneys.
All these complications start from the very beginning of T2DM occurrence and ultimately affect over 10-50% of diabetics after 10 years of not meticulously controlled blood glucose levels.
Graph: HbA1c and incidence of macrovascular (CAD) and microvascular disease.
It is vary glaringly apparent that only, and only if the HbA1c is maintained at 5.7 or so, will the microvascular and macrovascular consequence be the least due to T2DM i.e. ~5% and ~15% respectively. If the current goal set by ADA of 7% is taken as a target then the incidences of both these consequences double! Hence, one needs to be wary of advice given and believing in Dr. Google sans basic understanding.
VEGETARIAN & VEGAN DIABETICS - HIGHER RISK OF PERSISTENT UNCONTROLLED HYPERGLYCEMIA
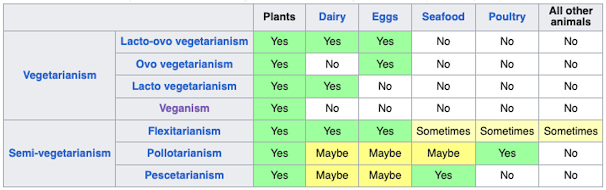
70-80% of Indians are non-vegetarians but they essentially follow a flexitarian diet, wherein meat, etc. is a small and infrequent component of everyday meal intake, and they are never truly daily consumers of animal food items.
Table: Intake of food items by Indians depending on their dietary following.
Hence, Indians generally are, at the best, semi-vegetarians. This is the reason why 84% of the vegetarian Indians and even 65% of those non-vegetarian are protein-deficient. What is replacing the necessary and recommended protein component of diet are the carbs, whether it is the vegetarian, vegan and even in those who are (pseudo-)non-vegetarian. 70% of Indian vegetarian and vegan diets are essentially carbs!
The excess carbs that the body cannot accommodate in muscles beyond their maximum storage capacity are diverted to liver for conversion to triglycerides. The resultant fatty liver results in hyperinsulinemia. It is because of hyperinsulinemia there is overproduction of very low-density lipoprotein (VLDL), higher triglyceride levels (hypertriglyceridemia) as well as excess mfg. of more small, dense LDL which are more harmful to the arteries in terms of plaque formation. Due to fatty liver, more triglycerides are transferred to the HDL (high density lipoprotein) particles and hence their content of friendly cholesterol (HDL-C) is curtailed. This is the explanation of the characteristic triad of T2DM.
Hence, the key lies in lowering the high insulin levels if not only the complications of T2DM but diabetes per se is to be theoretically reversed.
CARBS & GI
In general, foods that cause blood sugar level to rise the most are those that are high in carbohydrates. The glycemic index (GI) of carbs items also dictate which cause more glucose to be absorbed from a particular food item. The University of Sydney has defined foods as per their GI values:
- GI of over (>) 70 - "high GI foods"
- GI value of between 56 and 69 - "mid-range GI foods"
- GI value of 55 or under (<) - "low GI foods"
Thus, it is a foregone conclusion that most Indian prepared foods will have a moderate to high GI. Chicken, beef, fish and eggs all have a GI of zero because they contain zero or very small amounts of carbs and hence have a minimal effect on blood sugar levels.
CONCLUSIONS
Plant-based nutrition seems to have gained increasing popularity and represents a growing social movement. Female gender, younger age, lower BMI (body mass index - criteria for overweight and obesity), higher depression scores as well as increase in eating disorder-related psychopathology are significantly associated with vegetarian/vegan diets.
India ranks as the nation with the largest population of vegetarians (estimated to be 300-400 million) in the world. At the Third International Congress of Vegetarian Nutrition the tradition of vegetarianism in India was explained as being at least 3000 years old. The tradition is deeply rooted in religion (i.e., Hinduism, Vedic teachings) and continued in rural India out of economic necessity. Early vegetarian diets emphasized cereals, brown rice (“parboiled” with the husk), pulses, roots and tubers and also included fermented milk (i.e., curd) as a protein source. Age-old Vedic practices also promoted the use of fresh sprouting seeds such as mung bean and green gram, with minimal cooking of plant foods and the use of ground green bioingredients (“cooking without fire”). Hence, vegetarianism originally was not about promoting excessive harmful carbs intake - it meant consuming enough proteins and laid emphasis on consuming carbs with low GI.
However, in today’s times, carbs in excess, and of high GI values, are consumed in vegetarian, vegan as well as, to a lesser extent, in flexitarian diets. They are the culprits in causing insulin resistance and hyperinsulinemia followed by the various complications of T2DM if the hyperglycemia is not strictly checked and blood glucose maintained just like a normal individual's reading i.e. both fasting and PP levels of <110 mg/dL. Replacing carbs with non-vegetarian offers a logical option since these foods have a zero GI because of lack of significant amounts of carbs. Everyone dreams of wishing away his diabetes but only restricting carbs to 20 gms per day can be the key and a hope for the same.
Stay tuned for more on carbs associated pitfalls! Carbs are UGLY. Be Wary!
DR R K SANGHAVI
Prophesied Enabler
Experience & Expertise: Clinician & Healthcare Industry Adviser










Comments
Post a Comment